Myasthenia Gravis Stem Cell Therapy
autoimmune
Stem Cell Treatment
Stem Cell Therapy for Myasthenia Gravis: What You Need to Know
Why Myasthenia Gravis Is So Challenging
Myasthenia Gravis (MG) is an autoimmune condition that disrupts communication between your nerves and muscles. Normally, nerves send signals to muscles to make them move. In MG, your immune system mistakenly attacks the connection points-called neuromuscular junctions-where these signals are received.
The result is muscle weakness that gets worse with activity and improves with rest. But "rest more" isn't a real solution when life demands you keep moving.
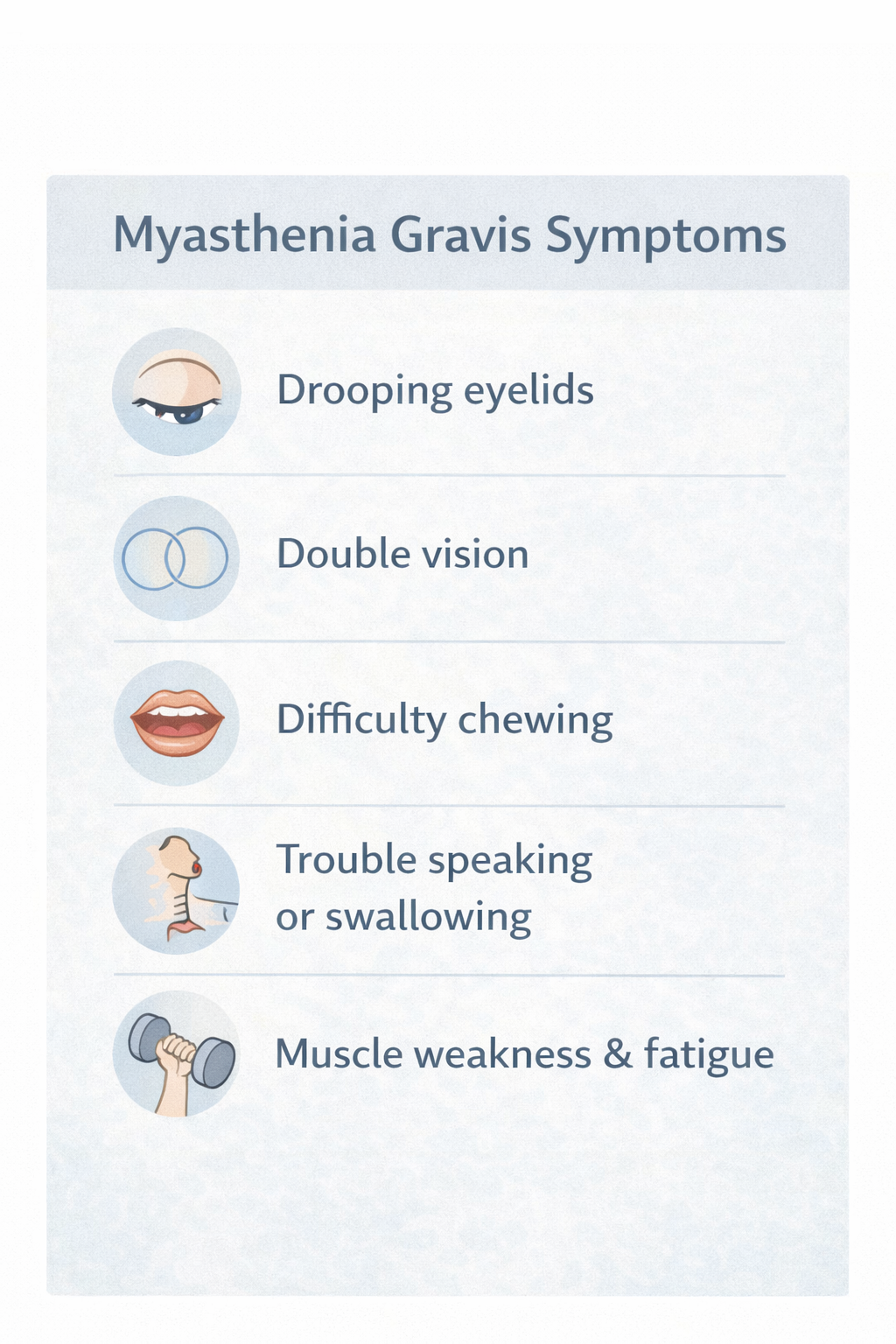
MG can affect almost any muscle, but commonly impacts the eyes (droopy eyelids, double vision), face (difficulty smiling, chewing), throat (trouble swallowing or speaking), and limbs (difficulty walking or lifting). For some people, it can affect breathing muscles, which requires immediate medical attention.
Symptoms vary from day to day-sometimes hour to hour. Medications, thymectomy, and other treatments help many people, but some continue to struggle with symptoms that limit their quality of life.
If standard treatments haven't given you the relief you need, stem cell therapy may be worth understanding.
What Stem Cell Therapy Is (Plain English)
Stem cell therapy is a treatment that aims to support your body's natural repair and regulation processes. The cells used are adult mesenchymal stem cells (MSCs) derived from carefully screened placental tissue. These are not embryonic stem cells.
The old thinking about stem cells was simple: inject new cells, they become new tissue. New muscle. Like replacing worn parts.
The current understanding is different-and actually more promising.
While stem cells may develop into new tissue cells to a limited degree, that's not their main value. What makes them therapeutically useful is their ability to coordinate and support your body's own healing-and in autoimmune conditions like MG, to help calm an overactive immune system.
What stem cells actually do:
- Release anti-inflammatory signals that may help quiet the immune attack on your neuromuscular junctions
- Support muscle repair by releasing growth factors that encourage healing
- May improve blood flow and nutrient delivery to affected muscles
- Help modulate (not suppress) immune function-rebalancing rather than shutting down
- Aim to create conditions where your muscles can recover and function better
Think of stem cells less like replacement parts and more like project managers. They assess the situation, calm the chaos, call in resources, and help coordinate repair. In MG, the "chaos" is your immune system attacking your own nerve-muscle connections. Stem cells may help restore order.
This is also why some patients notice improvement in the weeks following treatment. Early benefits often reflect reduced inflammation. Longer-term improvements may reflect actual tissue repair and improved muscle function.
Who This Is (and Isn't) For
May be appropriate if you:
- Have been diagnosed with Myasthenia Gravis and continue to experience symptoms
- Have tried standard treatments (medications, thymectomy) without sufficient improvement
- Want to explore options that may support muscle health and immune modulation
- Are in stable condition (not in myasthenic crisis)
- Have realistic expectations about timeline and outcomes
Probably not appropriate if you:
- Are experiencing myasthenic crisis or severe respiratory symptoms (seek emergency care)
- Haven't yet tried standard MG treatments
- Have other unstable medical conditions that need to be addressed first
- Are looking for a guaranteed cure
How Stem Cells May Help With Myasthenia Gravis
Calming the Immune Attack
The problem: MG is fundamentally an autoimmune condition. Your immune system produces antibodies that attack acetylcholine receptors at your neuromuscular junctions-the places where nerves communicate with muscles. This ongoing attack is what causes your muscle weakness.
What you experience: Muscle weakness that worsens with use, fatigue, difficulty with repetitive movements.
How stem cells may help: Stem cells release anti-inflammatory signals (like IL-10) that may help calm the overactive immune response. Rather than suppressing your immune system entirely (like some medications do), stem cells appear to help modulate it-encouraging it to stop attacking your own tissues while still functioning normally. Less immune attack on your neuromuscular junctions may mean better nerve-muscle communication and less weakness.
Supporting Muscle Repair
The problem: The ongoing immune attack in MG damages not just the neuromuscular junctions but can also affect muscle tissue itself over time. Muscles that aren't receiving proper nerve signals can weaken and atrophy.
What you experience: Progressive weakness, muscle fatigue, difficulty maintaining strength even with rest.
How stem cells may help: Stem cells release growth factors like IGF-1 (insulin-like growth factor) and FGF (fibroblast growth factor) that support muscle cell health and repair. They may help recruit your body's own repair cells to damaged areas. By creating conditions that favor muscle maintenance and repair, stem cells aim to help your muscles stay stronger and more resilient.
Improving Blood Flow to Muscles
The problem: Muscles need good blood supply to function well and heal. Chronic inflammation and immune activity can compromise circulation to affected tissues.
What you experience: Fatigue, slow recovery after exertion, muscles that tire quickly.
How stem cells may help: Stem cells release VEGF (vascular endothelial growth factor), which may support the growth of new blood vessels-a process called angiogenesis. Better blood supply means more oxygen and nutrients reaching your muscles, potentially improving their function and recovery capacity.
Reducing Overall Inflammation
The problem: Beyond the specific immune attack on neuromuscular junctions, MG involves systemic inflammation that can affect your energy levels, healing capacity, and overall well-being.
What you experience: General fatigue, feeling unwell, slow recovery from flares.
How stem cells may help: Stem cells have broad anti-inflammatory effects. By releasing various signaling molecules that calm inflammatory processes throughout the body, they may help reduce the overall inflammatory burden. Less systemic inflammation may mean more energy, better healing, and improved quality of life.
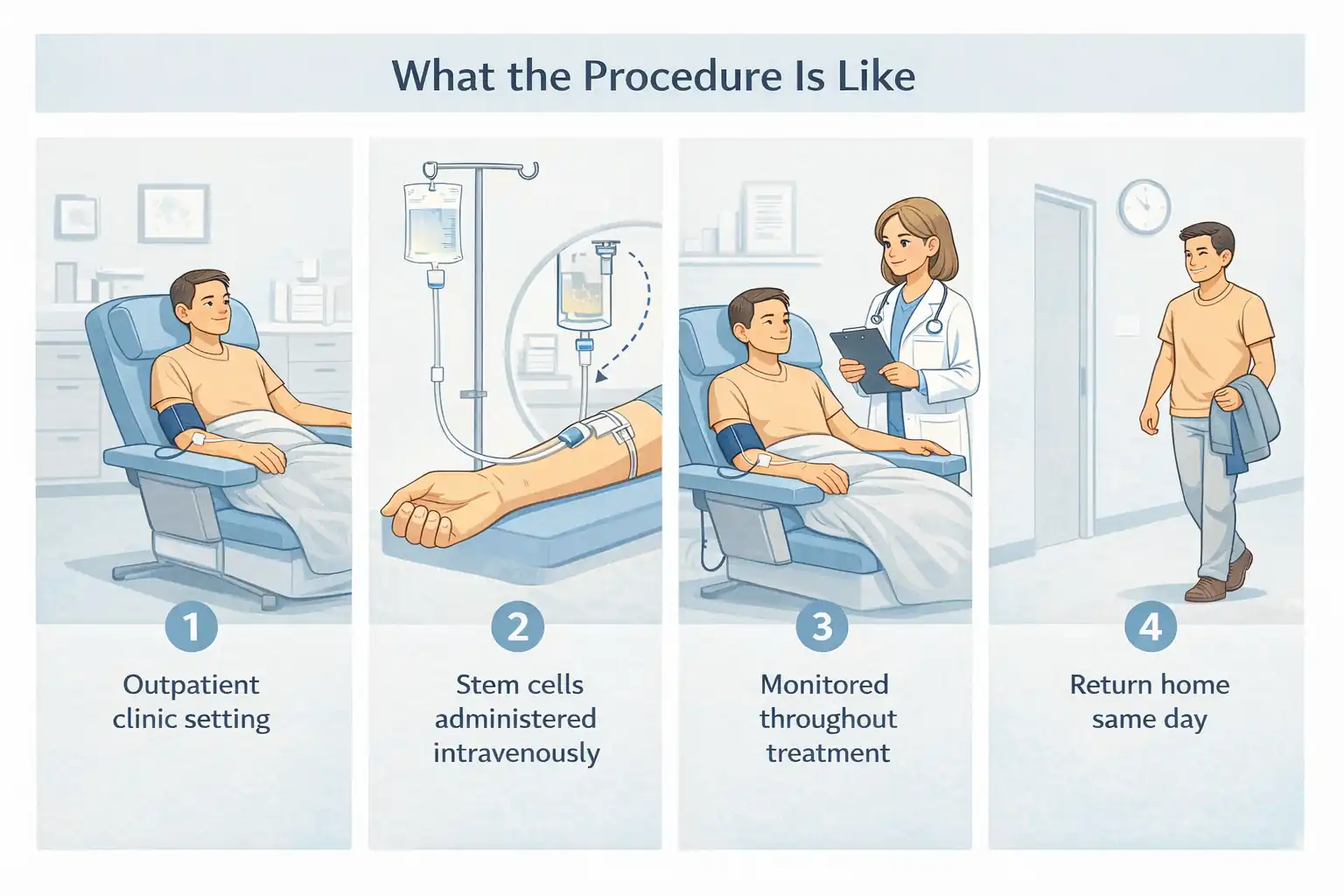
What the Procedure Is Like
Stem cell therapy for Myasthenia Gravis is performed as an outpatient procedure. The treatment is administered intravenously, allowing the stem cells to circulate throughout your body and reach affected tissues.
Here's what to expect:
1. Consultation and evaluation The medical team reviews your MG history, current medications, symptom patterns, and overall health to determine if stem cell therapy is appropriate for your situation.
2. Stem cell preparation We use mesenchymal stem cells derived from carefully screened placental tissue. These cells are processed and prepared for administration.
3. Treatment administration Stem cells are administered intravenously in a controlled clinical setting. The procedure typically takes 1-2 hours. You'll be monitored throughout for comfort and safety.
4. Post-treatment Brief monitoring period, then home with specific instructions for follow-up care. Most patients can return to normal activities within a day or two.
How is this different from standard MG medications?
Standard MG treatments work in different ways-cholinesterase inhibitors improve nerve-muscle signaling, immunosuppressants reduce immune activity, and thymectomy removes the thymus gland. These are important and you should continue them as directed by your neurologist.
Stem cell therapy takes a different approach: rather than blocking specific pathways, it aims to help rebalance and modulate your immune system while supporting muscle repair. It's designed to work alongside your existing treatment, not replace it.
Recovery Timeline: What to Expect
Stem cell therapy for MG works gradually. Your immune system and muscles need time to respond. Be patient.
First 24-48 hours Rest and take it easy. Some patients feel fatigued after treatment. This is normal.
Weeks 1-4 Continue your normal MG medications as prescribed. Some patients notice early improvements in energy or muscle endurance; others don't yet. Both are normal. The stem cells are beginning their work.
Months 1-3 Immune modulation and anti-inflammatory effects may become noticeable. Many patients report improved muscle strength, less fatigue, and better tolerance for activity during this window.
Months 3-6 This is often when more significant improvements occur. Muscle function may continue to improve. Some patients find they can do more before experiencing weakness.
Months 6-12 Peak benefits typically appear for those who respond well. Improvements tend to stabilize.
Important: Individual responses vary considerably. MG severity, how long you've had the condition, your overall health, and other factors all influence outcomes. Some patients see meaningful improvement; others experience more modest changes. This therapy works alongside-not instead of-your standard MG care. Continue working with your neurologist throughout.
How This Compares to Other Options
The key difference: Standard MG treatments are important-they help manage symptoms and reduce disease activity. Cholinesterase inhibitors improve signaling but don't address the immune attack. Immunosuppressants reduce immune activity but suppress function broadly. Thymectomy helps some patients significantly but requires surgery.
Stem cell therapy aims to help rebalance immune function while supporting muscle repair-a different approach that may complement your existing treatment.
Bottom Line: Is This Worth Considering?
Stem cell therapy for Myasthenia Gravis isn't a guaranteed fix. It's one option among several-and it's not right for everyone.
It may be worth considering if:
- You have MG and continue to experience symptoms despite standard treatments
- You want to explore options that may help modulate your immune response
- You're looking for approaches that support muscle health, not just symptom management
- You're in stable condition (not in crisis)
- You're willing to give your body time to respond (weeks to months)
- You have realistic expectations about outcomes
The proposed mechanisms are biologically plausible-stem cells do appear to have immunomodulatory and anti-inflammatory properties. The safety profile appears favorable when properly administered. Some patients report meaningful improvement in strength, energy, and quality of life.
But "some" isn't "all." Results vary based on disease severity, how long you've had MG, your overall health, and factors we don't fully understand yet. This is an evolving field.
If you're interested, a consultation can help determine whether this approach makes sense for your specific situation-and set realistic expectations. This therapy works alongside your standard MG care, not instead of it. Continue working with your neurologist.
Individual results vary. No outcomes guaranteed. For educational purposes only-not medical advice. Consult a qualified provider and your neurologist to determine if appropriate for you. Statements not evaluated by FDA or COFEPRIS.
Treatment
- Medical consultation
- 300 million Stem Cell IV
- Brain IV + High DoseVitamin C + others as need
- Full blood panel
- Recommended supplements to take.
- Recommendation on things to do to enhance wellness.
Start Today
We invite you to embark on this transformative journey with us through our certified stem cell therapies, a premier treatment option. A stem cell specialist will guide you through the entire process, explaining the program, benefits, and what to expect during and after the procedure. If you have any questions, suggestions, or would like to schedule a consultation, please feel free to reach out. Our dedicated team is here to provide you with the support and information you need to make informed decisions about your health.
